I’m now into my third life on planet Earth.
In ancient civilizations, life expectancy was thirty years.
In 1920, it was forty years.
Today, in developed countries, we can live to the age of forty twice, hence an “extra life,” as Steven Johnson termed it.
There has been a dramatic rise in life expectancy in the last hundred years. We’re surfing the crest of this fantastic wave:

Sadly, some of us still perish in infancy, stupid teen years, or even more stupid—war years.
But as each decade rises like the morning sun, our lives grow brighter and longer, mainly due to better sanitation, nutrition, vaccines, antibiotics, and medicine in general.
It’s this last, medicine in general, that keeps our extra life safe.
So many of us are here to read my humble writings, thanks to medical breakthroughs that have become routine.
I spoke with a man whose journey through advanced medical treatments was encouraging. You can see my previous essay about him here: in March 2024.
He said back then, only 13% of stage four cancer patients survived for five years. He had five years and three months of survival at that time.
Now he has seven years of survival under his belt.
They don’t have survival percentages after five years.
But Paul’s survival, though remarkable, is not singular. He said there are some he knows who have survived ten to fifteen years.
Paul’s journey was long and arduous. You can see the details of his experience below in an article by Julia Brabant of the Seena Magowitz Foundation, so I won’t repeat them.
But I will give you some insight about Paul that is not in the article.
Paul gained extensive experience in cancer therapy. He became an astute student, asked questions, suggested valid alternatives, and persevered.
Most importantly, he wants people to know cancer is not a death sentence. He wants to instill hope in all who have cancer.
Sometimes Paul went against medical advice, feeling that the effects of chemo weren’t worth it. He stopped after two days of it.
He tried alternative treatments like Lipoic Acid, which is not covered by insurance. But he feels his out-of-pocket investment in a longer life paid off.
He was also blessed to have been under the care of some competent and caring people, like the physicians of Weill Cornell Medical in NYC, Dr. John Ng and Dr. Steve Lee. Paul said, “Those are my guys; they saved my life.”
Paul said he was about to get more radiation, but Dr. Ng, ever diligent, said, “I’m not comfortable doing this because you’re right up there, on the cusp of the max of radiation, and it’s right in the same area. I’m concerned we could do damage to your bowel. So if there’s something else that maybe we can figure out that you can do. And we did”
About Dr. Steve Lee, Paul said, “I trusted him with my life; he’ll talk with me on the phone for a half hour or forty minutes. What doctor does that? Nobody.”
Dr. Lee asked Paul to call him Steve. Paul said, “Steve will call me in his car on his free time. We email back and forth. He’s the best doctor in the world.”
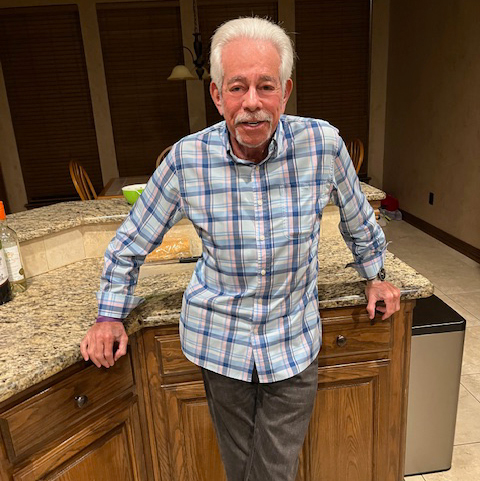
Despite cancer, Paul is enjoying his second life. He does have good days and bad. But he still plays golf.
Last year, he went to Italy and a fourteen-day cruise. He came home with swollen feet, but he said, “I made that trip, I really wanted to.”
He is also still an active board manager on his condo board. He’s unsinkable.
Paul educated me in many ways through his experience. He said it is common knowledge that alcohol damages the liver, but alcohol injected into a tumor shrinks it.
Paul has a fantastic attitude, and I think it plays a good part in his success. You might recall from my first essay on Paul that his career was in stand-up comedy. He can’t help but stay in that role.
He said, “Remember that Seinfeld episode where George, just out of a Hampton’s pool, was so concerned about apparent shrinkage?” Paul finished with a wide grin, “Well, shrinkage is a blessing for people who have cancer.”
Good night, folks. I love you, New York!
Yes, Paul loves life; he enjoys shore life. He said he loves sitting on the beach or his terrace listening to the crash of waves and the call of gulls.
That’s fantastic; Paul Suntup’s earned the extended joys of his second life. And he wants to show others they can too.
If someone wants to reach Paul they can contact the Pancreatic Cancer Action Network, where he volunteers, PANCAN, 877-2-PANCAN, and request to be in contact with Paul Suntup. PANCAN will give them an email through which they can contact Paul Suntup.
Be well,
Leebythesea
Here is the Julia Brabant article:
Paul Suntup’s Journey with Hope:

Donate
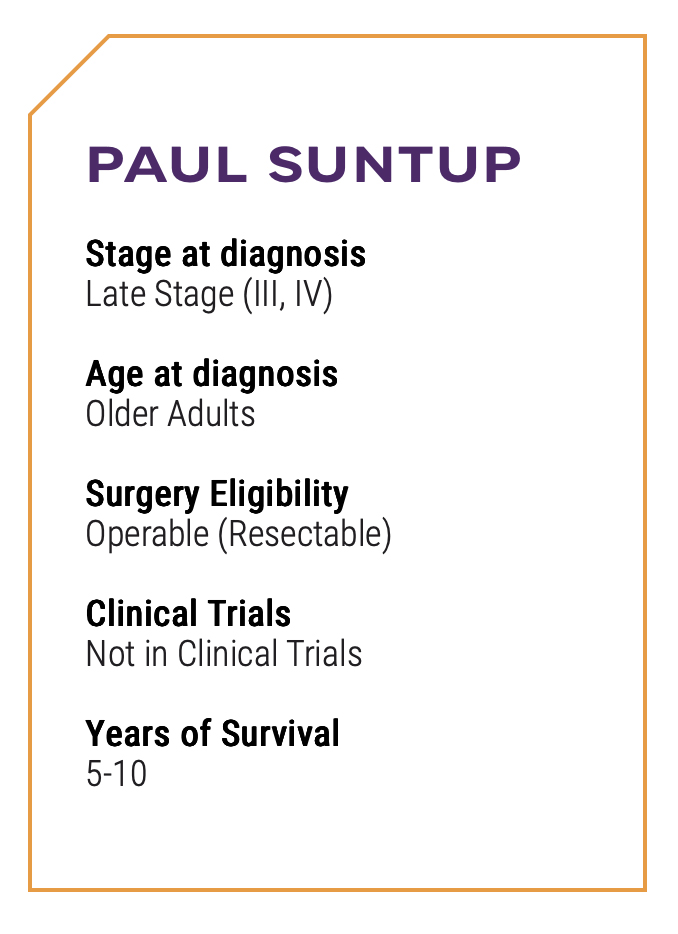
PAUL SUNTUP
Written By: Julia Brabant September 2025
Living with Acinar Cell Carcinoma: How One Man Turned a Rare Diagnosis into Hope
When Long Beach, New York’s Paul Suntup started having painful pancreatitis attacks, they proved a blessing in disguise, with the pancreatitis ultimately paving the way for Paul’s diagnosis of acinar cell carcinoma, a rare form of pancreatic cancer. He faced a similar catch-22 later in his cancer journey, when his BRCA2 gene mutation, which placed him at a higher risk for pancreatic cancer, also opened up new doors and treatment options that might have otherwise proved inaccessible.
Paul’s pancreatitis bouts began in 2017, and he visited the local emergency room, where doctors noticed high lipase and amylase levels. They wanted to admit him, but Paul refused. About a month later, he had another major pancreatitis attack. This time, he showed up with an overnight bag.
Doctors expressed concern about the ongoing bouts of pancreatitis, noting that every attack increases the odds of pancreatic cancer.
“That hit me between the eyes,” Paul said. “We were talking about pancreatitis, and then all of a sudden, we were talking about cancer.”
Paul stayed in the hospital until his lipase levels came down, returning for follow-up scans every few months. About a year later, doctors saw something concerning, leading to an ERCP and a biopsy to confirm the presence of cancer. Doctors weren’t initially sure what kind, though, and it took several labs to land at the diagnosis of acinar cell carcinoma.
In retrospect, Paul recalls having stomachaches for years. He’d undergone scans and tests to try to figure out the cause, but nothing ever came up. This is not uncommon with pancreatic cancer, which can be difficult to detect at its early stages.
Paul’s diagnosis left him with a difficult decision to make. He was going to have surgery – that much he knew. What he had a harder time deciding was whether to have chemotherapy, given the specifics of his rare form of cancer and the recommendations of various doctors.
He’d seen one oncologist who recommended he not have chemo post-surgery. Other doctors agreed, stating they weren’t sure it would be beneficial in Paul’s particular case. Some doctors he saw weren’t even familiar with acinar cell carcinoma, and since Paul, himself, preferred not to have chemo if he could avoid it, he opted to forgo it – for the time being.
Paul underwent a distal pancreatectomy and splenectomy in December of 2018, after a gastroenterologist put him in touch with a world-renowned cancer surgeon who’d agreed to take his case. The doctor believed he could remove all of Paul’s tumor laparoscopically. After the procedure, he gave Paul “the best post-op report one can have.” All of his margins were clear, and they’d also tested 22 lymph nodes for signs of cancer, all of which also came back negative.
After recovering, Paul eased back into life. After receiving an “all clear” at the three-month mark, he traveled to an all-inclusive resort in Costa Rica to celebrate. Yet, at his next follow-up three months later, 23 new tumors had appeared on Paul’s liver. His medical team was shocked, as was Paul.
He asked his oncologist how probable it was that he’d live another 10 years, which the oncologist thought was unlikely. Paul then questioned if he might make it another five years, but was told that this, too, was doubtful. When he asked about his chances of surviving for another three years, his doctor stopped him, noting that he’d rather not put a specific number or prediction on things at this point.
Paul made the difficult decision to start chemo. However, he stopped taking FOLFIRINOX shortly after, choosing instead to pursue other treatment options that may have more minimal side effects. He started getting alpha lipoic infusions (also called ALA IV treatments) after hearing about a doctor in New Mexico who was administering them to patients alongside low-dose naltrexone, a medication often used to treat opiate and alcohol misuse disorders, with much success.
Paul’s tumors reduced in size for about five months, which Paul believes could be due to the chemotherapy, the ALA IV and other treatments, or a combination of it all. Yet, at that five-month mark, his tumors suddenly started growing, putting him back in a position of uncertainty.
While Paul pondered next steps, he got something of a “gift” for his 70th birthday. The U.S. Food & Drug Administration approved a “PARP inhibitor,” a type of targeted therapy treatment, called LYNPARZA, for people with certain forms of pancreatic cancer who also had the BRCA2 gene mutation – which Paul did. Within about two weeks, he had the medicine in his house.
Everything worked well for about 10 months, with all tumors shrinking in size. The LYNPARZA led to side effects for Paul that included anemia, so he went off of it for about three weeks before resuming it, but at about two-thirds of his original dose. It wasn’t as effective this time, so Paul stopped taking it, instead opting to have something called a “Y90 radioembolization” treatment. The treatment involves finding out which blood vessels within the liver are feeding the tumors and injecting radiation into them.
Paul also had Stereotactic Body Radiation Therapy, or SBRT, to treat tumors on his liver and peritoneum. Once tumors appeared on his peritoneum, Paul’s oncologist suspected his condition might be systemic and wanted to treat it as such, rather than relying on targeted therapy. Paul’s oncologist also wanted him to start chemotherapy again. Instead of going back on FOLFIRINOX, Paul opted to have “metronomic” chemotherapy, which involves giving lower, consistent doses over a longer period of time.
Because of Paul’s BRCA2 mutation, he was eligible for a platinum-based chemotherapy. He began taking Xeloda and capecitabine alongside Oxaliplatin infusions, with platinum-based drugs like Oxaliplatin often proving more effective for people with the BRCA2 gene and metastatic pancreatic cancer. This combination didn’t work in Paul’s case, though, with two tumors doubling in size and a new one appearing while he took it. He then opted for SBRT to treat those tumors, which was successful.
Those three tumors still appear on scans, but Paul’s doctor has seen no change in their size over the last few years and suspects they are “dead.” Paul also developed several other tumors, including one on the right rectus muscle in his abdomen. He underwent surgery to remove it, with his doctor confirming he had clear margins in the aftermath. Paul also had two new tumors in his liver, which doctors wanted to treat using “histotripsy,” a non-invasive ultrasound-guided technology used to destroy cancer cells without using radiation.
However, the technology has some drawbacks, one of which is that the ultrasound doesn’t pick up tumors in the liver or pancreas as easily as, say, an MRI. If it doesn’t identify the tumors, it can’t administer the treatment.
Such was the case for Paul, so his team turned to plan B for one of his tumors, opting for something called a “microwave ablation.” A microwave ablation is another minimally invasive treatment that uses heat created through microwave energy to destroy tumors. For the other tumor, Paul had an “alcohol ablation,” which involves injecting alcohol into a tumor or tissue to dehydrate and kill the cells.
“Interesting, right?” Paul said. “Alcohol kills your liver, but it can also kill tumors.”
At Paul’s most recent checkup, a CAT scan identified some spots on his rib. This didn’t particularly surprise Paul, as he’d been dealing with ongoing pain in the area for quite a while. His care team believed the spots were likely small fractures, rather than cancer, and that the remaining tumors Paul had were now either dead or gone. As a result, his radiologist told him he was “NED,” meaning he showed “no evidence of disease.” While this was great news for Paul, he’s well aware of the risk of a recurrence, so looks ahead to the future with cautious optimism. He also continues to experience some ongoing health issues, among them dizziness and lightheadedness, and he also bruises easily.
“I can’t keep track of where the bruises come from,” he said. “I’ve given up on trying to stay away from turning purple.”
Despite these complications, Paul feels lucky to have seven years in books since his diagnosis. He encourages everyone, especially those with family histories of cancer, to have genetic testing to check for mutations. He also hopes more doctors take mutations into account when recommending treatment for patients, as some can make people eligible for treatment options they might otherwise miss.
Paul also makes a point to share his story and volunteer for pancreatic cancer research organizations like PanCAN and The Lustgarten Foundation. He also shared his story as one of five survivors featured in the book, “How to Survive Pancreatic Cancer,” does live TV interviews to spread awareness about pancreatic cancer, and lends a listening ear to others diagnosed with the disease.
And when he fields calls from other people with pancreatic cancer, he tries to offer more than just empathy.
“I try to make light of things and use humor wherever I can,” he said.
Categories: surviving cancer